World Lichen Sclerosus Day
Written by Susan Miller, PT, DPT, and originally posted on lotuscorept.com.
January 17th was World Lichen Sclerosus Day but not many people know what this is or if they are experiencing symptoms. Let’s explore!
What is Lichen Sclerosus?
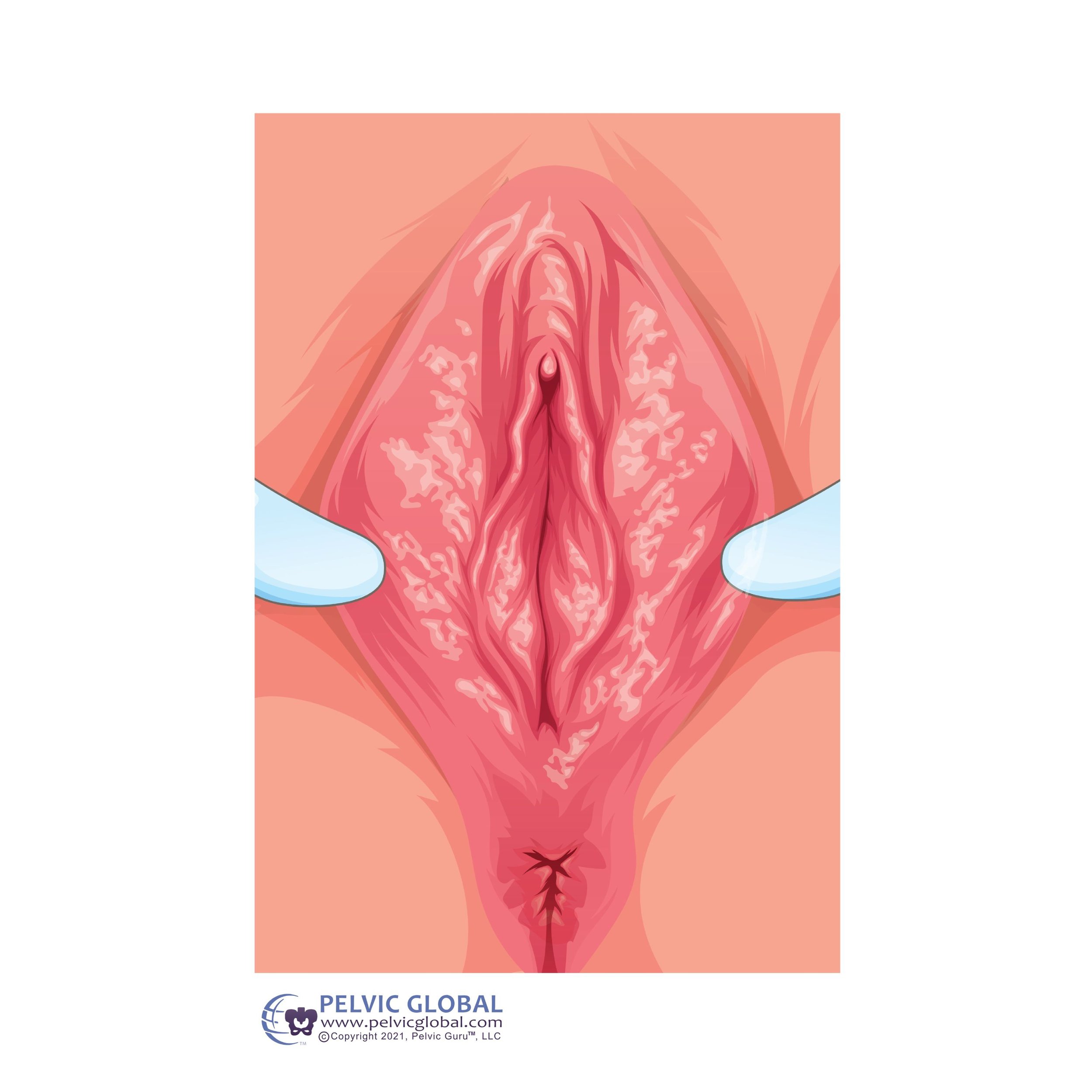
“Image used with permission from Pelvic Guru®, LLC www.pelvicglobal.com”
“Lichen Sclerosus is a chronic, inflammatory skin condition that primarily affects the anogenital epithelium in women.” (1)
Essentially , lichen sclerosus is a skin condition that causes skin alterations at the vulva. During an active flare, the vulva’s skin may undergo texture changes, color changes and bruising. Women can experience pain with intercourse, scarring, itching, fissures and bruising. Lichen Sclerosus has been identified as an autoimmune disease with a diagnosis delay of 4-6 years attributed to its overlapping symptoms with chronic pelvic pain. While post-menopausal women are commonly diagnosed, it can affect individuals of all ages. Recent research indicates its occurrence in menopausal women who are often overlooked due to symptoms resembling chronic pelvic pain, such as pain or tearing during intercourse. (1)
What are the symptoms?
Women commonly experience the following symptoms:
Irritation/burning
Pain with sex (Dyspareunia)
Scarring or architectural changes
Itching (Pruritus)
Fissures
Bruising
Difficulty achieving or not having an orgasm (Anorgasmia)
The most prevalent symptom is severe itching, typically observed in postmenopausal women (1). Young girls, before starting their periods, may also manifest symptoms, including itching, painful urination, constipation, vulvar pain, and bleeding (1). Early identification of these symptoms can facilitate the implementation of an effective treatment plan.
How do you diagnose and what is the treatment plan?
The initial step in diagnosis involves finding the right physician to determine if you have lichen sclerosus. This is crucial as it is often misdiagnosed as a yeast infection. A valuable resource for locating a physician can be accessed through the Lichen Sclerosus Support Network (https://www.lssupport.net/searchable-lichen-sclerosus-provider-database/) (2).
Clinical diagnosis involves observation or the extraction of a biopsy from vulvar tissues by a trained physician. Once diagnosed, the gold standard for treatment is ultra-potent topical corticosteroids (3,5). Additional medical treatments may encompass topical calcineurin inhibitors and platelet-rich plasma (PRP) injections (5). Each treatment should be tailored to the patient, emphasizing the importance of finding a knowledgeable physician early on who understands lichen sclerosus, enabling the right approach regarding dosing, application, and the type of medication.
What other treatments are helpful?
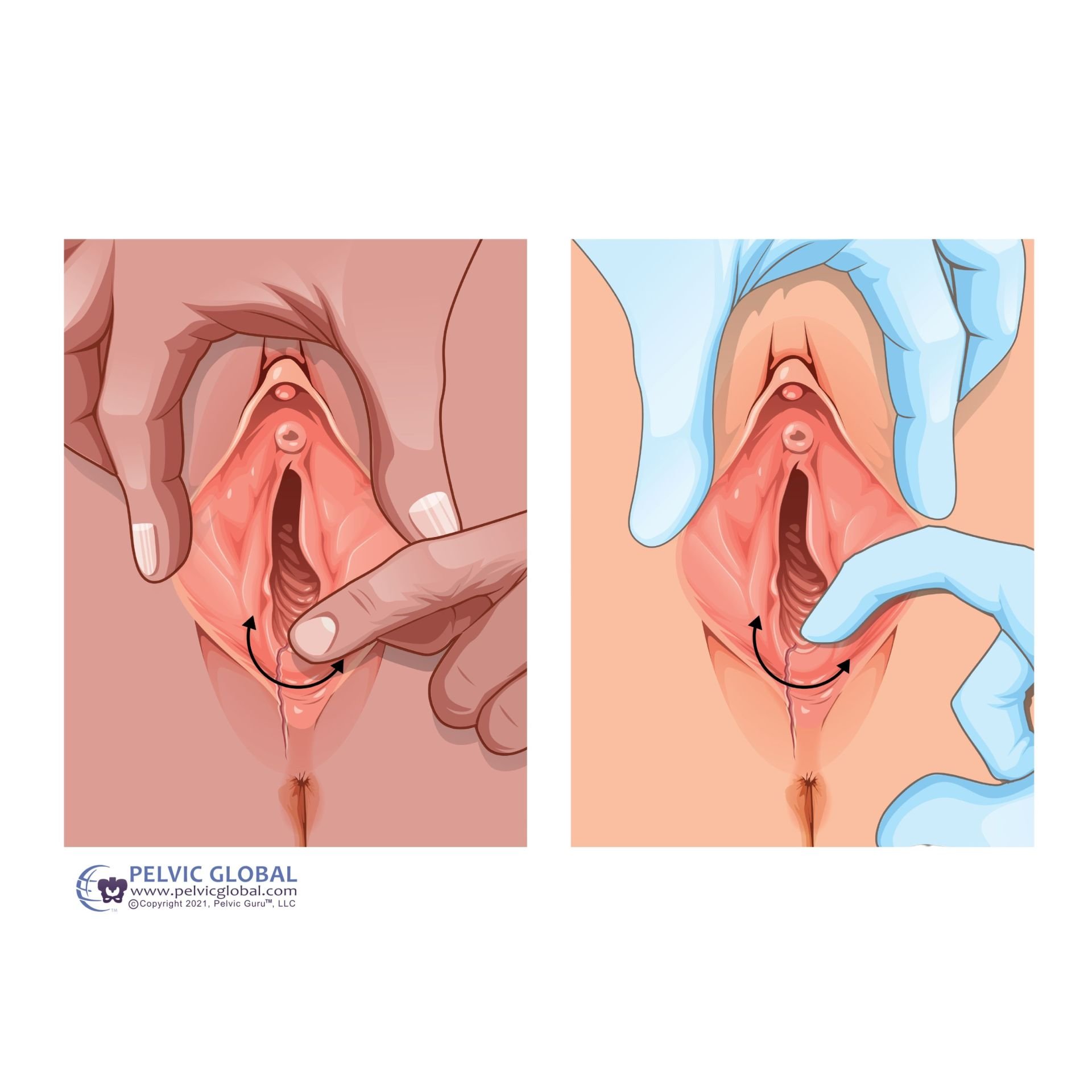
“Image used with permission from Pelvic Guru®, LLC www.pelvicglobal.com”
Energy-based therapies, such as photodynamic therapy, high-intensity focused ultrasound, and fractional CO2 laser therapy, have been researched. While these treatments appear promising, more research is needed to confidently recommend them for the treatment of lichen sclerosus (5).
Lichen Sclerosus can have physical and emotional impacts on women. Women may engage less in intercourse, grapple with self-image issues, develop fear, avoid the vulvar region, and experience pain (4). The inclusion of a mental health therapist, particularly one specializing in intimacy or sexual function, can offer strategies for fostering a healthy sex life and improving self-image. Additionally, pelvic floor physical therapy can be instrumental in alleviating physical symptoms.
How can Pelvic Floor Physical Therapy help?
Pelvic Floor Physical Therapists (PFPT) are specialists in the musculoskeletal system and its integration with the pelvic floor. Their primary role involves myofascial release of muscles, perineal massages, scar tissue mobilization, and providing education on dilator treatments. Another significant advantage of consulting a PFPT is their ability to identify skin changes. PFPTs serve as advocates, assisting individuals in finding the right professionals to address this condition.
If you are uncertain whether your symptoms align with Lichen Sclerosus, assemble a team of practitioners well-versed in diagnosis and treatment. This team may comprise a gynecologist, pelvic floor physical therapist, dermatologist, and mental health therapist.
Drop a comment or ask a question for more information.
Dr. Susan Miller PT, DPT, is a licensed pelvic floor physical therapist and the owner of Lotus Core Physical Therapy in Colorado. She welcomes both in-person and telehealth appointments for Colorado residents, as well as coaching calls for clients residing out of state. Book at www.lotuscorept.com.
Articles and Resources:
Krapf JM, Smith AB, Signa ST, Goldstein AT. Presenting Symptoms and Diagnosis of Vulvar Lichen Sclerosus in Premenopausal Women: A Cross-Sectional Study. J Low Genit Tract Dis. 2022. Jul1;26(3):271-275. doi:10.1097/LGT.0000000000000679.
The Lichen Sclerosus support network: https://www.lssupport.net/
Mautz TT, Krapf JM, Goldstein AT. Topical Corticosteroids in the Treatment of Vulvar Lichen Sclerosus: A Review of Pharmacokinetics and Recommended Dosing Frequencies. Sex Med Rev. 2022: 10(1): 42-52. doi:10.1016/j.sxmr.2021.03.006.
Govind V, Krapf JM, Mitchell L, et al. Exploring Pain-Related Anxiety and Depression in Female Patients With Provoked Vulvodynia With Associated Overactive Pelvic Floor Muscles. Sex Med. 2020; 8(3): 517-524. Doi. 10.1016/j.esxm.2020.05.009
Krapf, JM, Mitchell L, Holton MA, Goldstein AT. Vulvar Lichen Sclerosus: Current Perspectives. Int. J Womens Health. 2020;12:11-20. Published 2020 Jan 15. doi:10.2147/IJWH.S191200