The Long Road to Endometriosis
Written by Susan Miller, PT, DPT, and originally posted on lotuscorept.com.
The Long Road to Endometriosis
The endometriosis diagnosis has gained notoriety since the release of the documentary “Below the Belt.”(3) Special screenings started in 2022 with the film streaming on PBS at the end of June 2023 with multiple screenings still occurring today. The documentary follows four patients on their journey to understand their chronic pain and what it takes to find the correct treatment, a process that can take years for many women.
On average it can take 4 to 11 years to diagnose Endometriosis.(2)
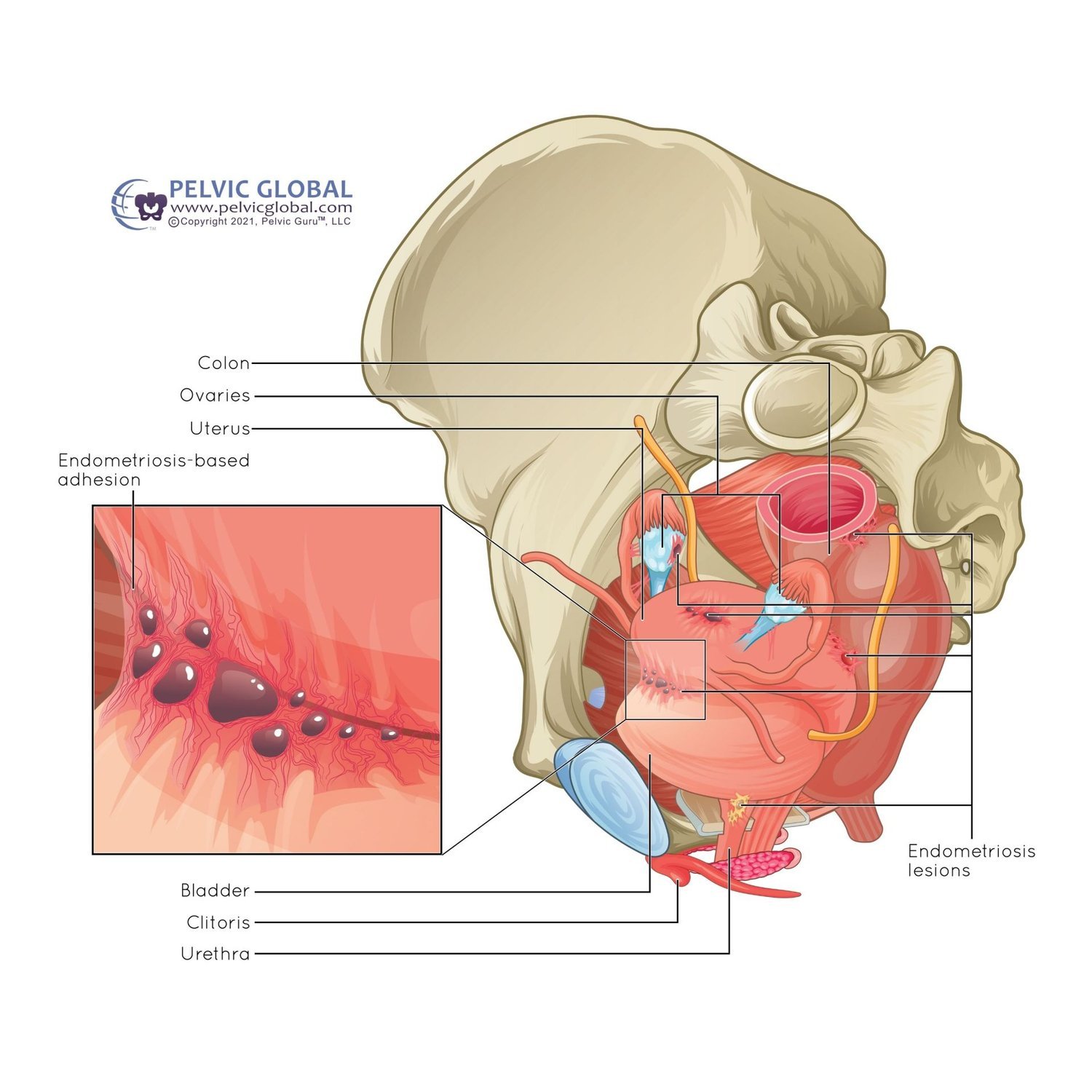
Endometriosis is endometrial tissue found outside of the uterine lining, typically in and around the pelvic cavity.(1) These tissues can adhere to the uterus, bladder, ovaries, fallopian tubes, rectum, and can even travel into the abdominal cavity, affecting the colon system and diaphragm. Unlike the tissues inside the uterus, endometrial cells found outside can cause pain, lesions, adhesions, and inflammation, contributing to debilitating pain during ovulation and menstruation.
“Image used with permission from Pelvic Guru®, LLC www.pelvicglobal.com as a member of the Global Pelvic Health Alliance Membership (GPHAM)”
In the image on the left you can see an example of endometriosis adhesions and lesions attached to the bladder.
According to research, the exact cause of endometriosis remains unknown, making it challenging to identity. Various theories have been proposed, including congenital, environmental, autoimmune, and allergic factors(1). It’s possible to have one of these factors without developing endometriosis. Endometriosis can lead to infertility, dyspareunia (painful sex), pain with menstruation, pain with urination, and bowel issues.(2) Endometriosis symptoms can affect their quality of life including relationships, work and social activities.
Why the Long Road?
Sadly, many women are dismissed when they bring up painful periods or heavy bleeding to their providers. They are also overlooked when reporting pain during intercourse, abdominal distension, abdominal cramping, fatigue, or difficulty with defecation. Another issue is that women can have a difficult time discerning what is normal for periods, even when their periods are disrupting their lives. Additionally, they may feel too embarrassed to discuss their pain levels and begin to withdraw from daily activities to cope.(4)
While women may feel dismissed or too embarrassed to bring up their symptoms, diagnosing endometriosis can be challenging due to overlapping symptoms with other gynecological conditions, such as pain with intercourse, painful bladder syndrome, painful periods, or bowel dysfunction.(4)
The gold standard for diagnosis is laparoscopic surgery with tissue biopsy for confirmation. However, technically, surgery is not necessary for an endometriosis diagnosis, as there is a push by experts to treat clinically if they suspect endometriosis.(6) Treating someone clinically can aid in identifying symptoms early and starting treatment sooner. Nonetheless, laparoscopic surgery can still be beneficial in cases of complexity. Other low invasive imaging tools can include MRI and transvaginal ultrasound.(6) Endometriosis is staged from I to IV, representing mild to severe, but this does not necessarily correlate with the severity of pain experienced.
Treatment typically includes surgical, pharmacological, or a combination of both. While there is no medication that slows down or reverses the disease process, hormonal and non-hormonal medications can assist in alleviating the symptoms and improving fertility.(5) Excision surgery is recommended if pharmacological treatment fails or to help increase the chances of fertility. Given the uniqueness of the endometriosis diagnosis, it is imperative to find a physician and support team that understands the different treatment options and what is best for you.
Outside of surgical or pharmacological management, many alternative therapies are available, including pelvic floor physical therapy. Physical therapy can play a vital role in various aspects of managing this disease, such as muscle and facial pain, post-operative management, scar mobilization, exercise prescription, bowel dysfunction, relaxation techniques, and/or tools such as vaginal dilators.(7) Most importantly, physical therapy can address the return to function. While pelvic floor physical therapists will have general techniques that are commonly used on each patient, not every technique will be beneficial on every individual. Working with your pelvic floor physical therapist to establish different tools to help reduce pain and improve function should be individualized to your needs.
The last critical step in completing a comprehensive treatment plan is to include mental health therapy. Mental health therapists play a crucial role in addressing the emotional and relational aspects associated with this diagnosis. This includes managing emotional distress such as anxiety or depression, developing coping strategies to adjust to living with endometriosis, focusing on pain perception for pain management, addressing relationship issues to improve communication skills and relationships, and implementing stress management techniques.
Endometriosis requires a multidisciplinary approach that integrates medical, psychological and physical interventions. By raising awareness, advocating for timely diagnosis and appropriate treatment, and providing comprehensive support, a team of professionals can assist you in improving your life while managing this debilitating condition.
Find out more about pelvic floor physical therapy and Susan Miller, PT, DPT by visiting Lotus Core Physical Therapy.
Resources:
Smolarz B, Szyłło K, Romanowicz H. Endometriosis: Epidemiology, Classification, Pathogenesis, Treatment and Genetics (Review of Literature). Int J Mol Sci. 2021 Sep 29;22(19):10554. doi: 10.3390/ijms221910554. PMID: 34638893; PMCID: PMC8508982.
Tsamantioti ES, Mahdy H. Endometriosis. [Updated 2023 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567777/
More information on “the Below the Belt” documentary can be found here: https://www.belowthebelt.film/
Ballard K, Lowton K, Wright J. What’s the delay? A qualitative study of women’s experiences of reaching a diagnosis of endometriosis. Fertil Steril. 2006;86(5):1296-1301. doi:10.1016/j.fertnstert 2006.04.054 )
Tsamantioti ES, Mahdy H. Endometriosis. [Updated 2023 Jan 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567777/
Hunt G, Allaire C, Yong PJ, Dunne C. Endometriosis: An update on diagnosis and medical management. BCMJ. 2021;63(4):158-163.
Wójcik M, Szczepaniak R, Placek K. Physiotherapy Management in Endometriosis. Int J Environ Res Public Health. 2022;19(23):16148. Published 2022 Dec 2. doi:10.3390/ijerph192316148